Haematology and Haemotherapy
Fundación Jiménez Díaz's Haematology Service was created in 1940 as a section of the Clinical and Medical Research Institute's Pathological Anatomy Department. Professor Jiménez Díaz brought in Dr Gregorio Paniagua to study haematopoiesis. In 1955, it was transferred to Clínica de la Concepción as an independent service. Three fundamental lines of work were developed under the direction of Dr Paniagua: a) Study of haematopoiesis and its pathology; b) Haemotherapy; and c) Haematology interconsultations. That is how one of Spain's pioneering Haematology services was formed.
In 1956, Dr José Sánchez Fayos and Dr Joaquín Serrano González-Solanes were appointed as assisting physicians in the Service. Both were sent to the U.S. for training in coagulation, haematopoiesis dynamics (Dr Sánchez Fayos), and immunohaematology and haemotherapy (Dr Serrano). On his return, Dr Serrano expanded the Blood Bank, started the fractionation of blood components, and set up the immunohaematology laboratory. Dr Sánchez Fayos added two of the clinic's internal physicians, Dr Enrique Villalobos and Dr Julio Outeiriño, to the team. Dr Villalobos set up the ferrokinetic and erythrokinetic studies. Dr Outeiriño expanded the haemostasis laboratory methodology, histochemistry, iron metabolism, diagnosis of haemoglobinopathies and thalassaemias, and initiated automation and quality control of routine tests. Also notable in this stage is Dr Teresa Calabuig’s role in Haematological cytology.
In 1980, the Service's clinical care activity, hitherto limited to patients and interconsultations from other services, was expanded with the acquisition of a Polyclinic and some beds in an Internal Medicine station. In 1983, Dr Antonio Escudero Soto was appointed as attending physician to the Department, taking charge of this clinical work, among other duties. Five years later, Dr Escudero moved to Gregorio Marañón Hospital, where Dr Elena Prieto Pareja took over his position and his duties, working years later alongside Dr Alejandro Román Barbero. Following Dr Serrano's retirement in 1991, Dr Luz Barbolla joined the Service and, with the collaboration of Dr Paniagua, reorganised and modernised the Blood Bank, set up aphaeresis programmes and started peripheral blood haematopoietic progenitor transplantation. The first transplant was performed in December 1993. Following Dr Barbolla's departure in 1996, Dr José Luis López Lorenzo, who is currently the Haematopoietic Progenitor Transplant Coordinator, joined the Blood Bank, which is now run by Dr Sol Sánchez Fernández.
Dr José Francisco Tomás was appointed Chief of Service after Dr Sánchez Fayos retired in 1998. This marked the start of a period of modernisation and expansion of the Service. At a clinical level, participation in protocols and clinical trials began at national level and the transplant area was strengthened, with the first allogeneic transplant being performed in 1998. Dr Carlos Soto de Ozaeta consolidated the area and took over as head of Hemacytometry and Cytology. Dr Pilar Llamas Sillero joined the group in 1998 following Dr Julio Outeiriño's retirement, continuing the work Dr Outeiriño had initiated in the field of thrombosis and haemostasis and developing the Thrombophilia Unit both clinically and in terms of laboratory practice. She currently holds the position of Head of the Haematology Service. Dr Llamas oversaw the setting up of the Haematological Molecular Biology Laboratory under Dr Carlos Blas López.
In 1999, the Haematology Service was strengthened with the incorporation of the Flow Cytometry methodology, led by Dr Cristina Serrano del Castillo. Finally, the Haematological Cytogenetics section was set up in 2000, and is currently directed by Dr Rocío Salgado Sánchez, from the Spanish National Cancer Research Centre (CNIO). In 2014, Dr Raúl Córdoba Mascuñano joined as Coordinator of the Lymphoma Unit, after completing his specific training in this pathology in Switzerland, Germany and the United States.
In 2014, the Haematopoietic Progenitor Transplant Unit started working alongside the Transfusion Service and the Haematopoietic Progenitor and Cell Therapy Laboratory to obtain JACIE accreditation (Joint Accreditation Committee of European Society of Blood and Marrow Transplantation - EBMT), which ensures compliance with the quality standards of the accrediting entities, presenting levels of excellence in care work.
The main mission of the Haematology and Haemotherapy Service is to provide comprehensive, personalised, quality medical care to patients with haematological diseases. Healthcare activity always places the patient at the centre of the process, following quality and efficiency criteria. Scientific and technical quality, along with Teaching and Research, are the key pillars that support healthcare activity.
It should be noted that our haemato-oncology activity is part of Oncohealth in the healthcare area. Also worthy of mention is our integration in cancer research as a group that is part of the IIS-FJD.
The Haematology Service is currently made up of 21 physicians, of whom 19 are specialists in Haematology and Haemotherapy, 1 is a specialist in Clinical Immunology, and 1 is a specialist in Oncohaematological Cytogenetics. The Haematology Service is accredited by the National Commission of the Haematology and Haemotherapy Speciality for medical residency training in Haematology and Haemotherapy, and currently has 8 resident physicians, 2 per year of training. A new resident position is expected to be approved in 2020.
Within the Service, the Cytogenetics, Molecular Biology, Flow Cytometry and Lymphoma Units are duly recognised and receive interns from different specialities from other centres. External interns have also recently been incorporated in the Haemostasis unit.
Service organisation
Haematology care activity is structured in different areas, as shown in the following diagram:
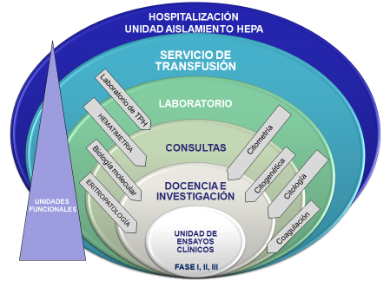
The different areas are as follows.
- Hospitalisation:
- Intensive hospitalisation and haematopoietic transplant (including the CART Therapy Multidisciplinary Unit).
- Haemato-oncology hospitalisation.
- Haemato-oncology day hospital.
- Outpatient Consultations:
- General haematology consultations.
- Specialist consultations.
- Care units.
- Anticoagulation and antithrombotic therapy unit.
- Lymphoma Unit.
- Myeloma and amyloidosis unit.
- Myeloid pathology and myeloproliferative syndromes unit.
- Haematogeriatric Unit.
- Transplant and cell therapy unit.
- Integrated diagnostic unit.
- Internal committees:
- Lymphoma committee.
- Myeloma and amyloidosis committee.
- Integrated diagnostic committee.
- Myeloid neoplasms committee.
- Transplant committee.
- Advanced therapies committee.
- Thrombosis committee.
- Laboratory:
All areas involved in Haematological diagnosis are represented in the HUFJD's Haematology Laboratory, for the study of both benign and haemato-oncological pathologies.
It has therefore been possible to form an Integrated Diagnostic Unit including the cytology, molecular biology, cytogenetics and flow cytometry departments, in collaboration with the Pathological Anatomy service.
- Haemacytometry laboratory.
- Haemostasis laboratory.
- Flow cytometry laboratory.
- Cytogenetics and molecular biology laboratory.
- Transfusion service and haematopoietic progenitor laboratory:
The transfusion service and the haematopoietic progenitor laboratory are found together at HUFJD, both under the direction of Dr Sánchez. This enables us to efficiently manage transfusion practices and patient identification in pre-transplantation, along with the mobilisation, cryopreservation and thawing of progenitor cells.
There is also good access to the Isolation Unit.
This department has been working with the Spanish Bone Marrow Donors Registry (REDMO) for the past two years, collaborating in extracting peripheral blood or bone marrow progenitors which are used for transplants at a national or international level.
- Preclinical Translational Unit in Experimental Haematology:
As befits a high-level hospital service, the Haematology Service is involved in intense experimental and preclinical research activity in the Experimental Haematology Laboratory at FJD's Health Research Institute, which carries out studies on the biology of different haematological diseases and on the activity of a range of experimental drugs, with a view to designing the most personalised treatments possible.
- Preclinical unit to advance the treatment of Acute Myeloblastic Leukaemia.
- Preclinical unit for tissue engineering applied to haematopoietic and/or leukaemic niche. Microenvironment and drug response.
- Coagulopathies preclinical translational unit.
- Preclinical translational unit for the genetic characterisation of myeloid neoplasms.
- Preclinical unit for immune effector cells applied to haematological malignancies. Development of new technologies.
- Clinical trials unit:
Haematology Clinical Trials Unit, the main goal of which is to develop and apply clinical trials from phase I (new drugs) to phase III (randomised studies). This Unit allows haematology patients to receive the best treatments and have access to new drugs.
Hospital Universitario Fundación Jiménez Díaz
Avda. Reyes Católicos, 2
28040 Madrid Madrid
© 2026 Quirónsalud - All rights reserved