Radiodiagnosis
RELEVANT FEMALE DISEASES
PELVIC VENOUS CONGESTION SYNDROME
Chronic pelvic pain is a very common problem in women, and one of its main causes is the presence of varicose veins in the pelvis . Interventional radiology plays a key role in treating pelvic varicose veins.
. Interventional radiology plays a key role in treating pelvic varicose veins.
The presence of these large dilated veins, known as varicose veins, causes localised pain around the uterus, ovaries and vulva. Your doctor may prescribe analgesics to reduce pain and hormonal treatments to relieve venous congestion.
Pelvic congestion syndrome can be treated with embolisation of these varicose veins by interventional radiology whenever these medications do not improve the problem.
This minimally invasive technique, which involves placing a needle inside the patient's veins, eliminates the blood flow to the diseased pelvic veins, therefore removing the pain.

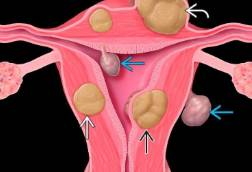
UTERINE FIBROIDS
Uterine fibroids are benign tumours that grow in the wall of the uterus, although the exact cause cannot be determined.
are benign tumours that grow in the wall of the uterus, although the exact cause cannot be determined.
These fibroids are fed by the uterine arteries, meaning their size varies; indeed, some fibroids can become very large, causing discomfort, pain or bleeding.
Uterine artery embolisation is a treatment option using interventional radiology, a minimally invasive technique that was initially used to treat postpartum haemorrhage, but which can now target the arteries of fibroids to reduce their size and alleviate symptoms.
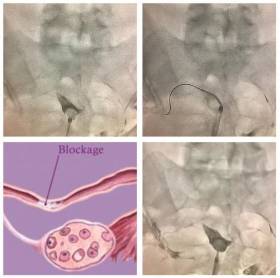
INFERTILITY DUE TO FALLOPIAN TUBE OCCLUSION
Fallopian tube occlusion is a very common cause of female infertility. We can open or recanalise these previously occluded thrombi to improve the likelihood of achieving a natural pregnancy. It is an outpatient procedure, requiring a little sedation.
is a very common cause of female infertility. We can open or recanalise these previously occluded thrombi to improve the likelihood of achieving a natural pregnancy. It is an outpatient procedure, requiring a little sedation.
We first perform a hysterosalpingogram and identify the tubal obstruction. We then advance to the occlusion point, using a guidewire and a catheter to navigate through the obstruction, reopening it in practically 100% of cases.
MAY-THURNER SYNDROME
May-Thurner syndrome (MTS) is related to the development of varicose veins and the formation of venous thrombosis in the left leg, caused by the left iliac vein (VII) being compressed between the right iliac artery and the spine. The veins and arteries sometimes intertwine, giving rise to compressive phenomena.
The exact origin of this compression is unknown, but it is very common in thin people, mainly women. One of the functions of fat in the body is to cushion some anatomical structures with others; thin people, having less retroperitoneal fat, are more prone to suffer from this syndrome.
What symptoms does it produce?
In May-Thurner syndrome, varicose veins may develop in the pelvis and legs, especially on the left. It can also generate venous thrombosis in the left leg, chronic oedema, malleolar hyperpigmentation (darkening of the skin in the ankle area), and lumbar pain.
What tests are necessary to diagnose the disease?
Firstly, non-invasive studies are requested from the vascular examination laboratory, whose most important tool is the Colour Doppler Ultrasound. With this technique we can see the structure, movement and function of the blood vessels in real time.
Another radiological study called iliocavography, which provides the definitive diagnosis, may be necessary on occasions. It consists of introducing a catheter through a vein in the elbow flexure, which is navigated to the pelvis with X-ray guidance. Once the veins to be studied have been cannulated, they are filled by injecting a contrast agent, allowing images to be obtained and even pressure gradients to be measured, providing valuable information on the compressive syndrome and its repercussions on the rest of the vessels. If the pelvic varicose veins have therapeutic indication, the treatment can be performed at this moment.
How can it be treated?
The procedure used in treating May-Thurner Syndrome is called angioplasty, and consists of introducing a special catheter at the exact point where the area of compression is located. Once there, a balloon is insufflated to dilate the compressed vein and a cylindrical mesh called a stent is fitted to prevent it from compressing again. This procedure does not require cuts or incisions on the skin, is performed with minimal sedation anaesthesia, and takes place in a digital angiography room.
RELEVANT MALE DISEASES
Erectile dysfunction is defined as:
Inability to achieve or maintain an erection firm enough for sexual intercourse, or
Total inability to produce an erection, or
Inability to produce a consistent erection, or
Tendency to maintain only brief erections.
Erectile dysfunction can have several causes, including altered nerve impulses in the brain, spinal cord, muscles, fibrous tissues, veins, and arteries of the penis. Vascular factors commonly underlie erectile dysfunction, which can stem from reduced arterial blood flow caused by occlusive pathology or venous leakage during erection, leading to the inability to sustain a satisfactory erection.
How is it diagnosed?
The predominant diagnostic imaging test is the penile Doppler ultrasound, which can often identify the arterial or venous origin of erectile dysfunction. Depending on the case, this may include injecting drugs into the corpora cavernosa, CT angiography (if arterial pathology is suspected), and/or diagnostic phlebography (if venous leakage is suspected).
Endovascular treatment
The therapeutic approach is usually through the skin (percutaneous). A catheter is used to access the pathological vessel and try to open it in the event of arterial dysfunction (stenting), or close it in the event of venous leakage (embolisation). Both techniques are usually performed under local anaesthesia, with minimal sedation and on an outpatient basis, allowing the patient to go home on the same day.
VARICOCELE
Varicocele is a very common problem in men, defined as dilation of the veins in the scrotum. The presence of these large dysfunctional veins can cause local pain, decreased sperm quality and quantity, and testicular atrophy. The presence of varicocele therefore decreases fertility.
Symptoms
Varicoceles are usually asymptomatic and patients will not experience any discomfort. It may occasionally cause scrotal pain and heaviness, which can vary from a vague, dull ache to a sharp pain, occurring more frequently after sports activities such as cycling. The pain often decreases with sitting.
Diagnosis
Regular diagnosis is based on clinical history, physical examination and confirmation with Doppler ultrasound.
Treatment
Treatment of varicocele is indicated when the patient is in pain, or there is a suspicion of secondary infertility or testicular atrophy. There are basically two therapeutic options: surgical repair, performed by the urologist, and the embolisation technique, performed by interventional radiologists.
Embolisation
The interventional radiologist will insert a catheter through a vein in the patient's forearm after applying a local anaesthesia. The catheter will be inserted into the testicular veins under X-ray guidance using iodinated contrast. The next step after confirming the presence of dilated veins (indicating a pathological condition) is to close them using agents based on metal coils or sclerosing foam.
Risks
The described risks associated with this technique include a small haematoma in the access area or a leakage of the embolisation material.
What is the procedure?
The procedure is performed under local anaesthesia and sometimes with minimal sedation; in no case will general anaesthesia be necessary. The patient will be able to go home about two hours after the operation, and will be regularly checked in follow-up consultations.
Recommended links:
Information for Patients: Interventional Vascular Radiology
Information for Patients: Uterine Fibroid embolisation
Information for Patients: Interventional Oncology
Hospital Universitario Fundación Jiménez Díaz
Avda. Reyes Católicos, 2
28040 Madrid Madrid
© 2026 Quirónsalud - All rights reserved